MTN’s approach to HIV prevention research
with pregnant and breastfeeding women
Clare Collins, MTN Communications
July 15, 2020
“If you are pregnant or nursing, consult your doctor before use.”
This disclaimer is commonly included in small print on the back of nearly every over-the-counter medication and in the package insert for most prescription drugs. Yet, if pregnant or breastfeeding women were to follow this advice, they probably wouldn’t get the answers they need. Little to no medical data exists for pregnant and breastfeeding women – in most cases, the studies were never conducted – leaving women and their health care providers in a difficult position.
Every day, countless numbers of pregnant and breastfeeding women are confronted with this dilemma, not knowing if a medication is safe to use – whether for a simple headache or something more serious. Evidence-based guidance on how to treat them safely and effectively is often not available because they are almost always excluded from research studies. In fact, most of what is learned about the safety of a drug during pregnancy and breastfeeding is obtained through surveillance registries that keep track of pregnancy complications and negative outcomes after drugs make it onto the market. If conducted at all, studies of drugs specifically in pregnant or breastfeeding women are typically completed years after they have been approved and made widely available.
“Many of the drugs we use in pregnant women have never been tested in pregnant women,” says Jeanna Piper, M.D., senior medical officer, Division of AIDS, National Institute of Allergy and Infectious Diseases (DAIDS/NIAID), part of the National Institutes of Health (NIH). “You may end up using the same dose of a drug you used in a non-pregnant woman, hoping it’s going to work, but you don’t really know. Sometimes it’s not going to be enough, sometimes it may be too much, and sometimes it may have effects on the baby.”
 Lacking data from clinical trials, many drugs simply are not recommended for use during pregnancy and lactation. This places the burden on health care providers to weigh the potential benefits and risks in prescribing drugs for pregnant and breastfeeding women who become sick or may need to continue treatment for a chronic illness.
Lacking data from clinical trials, many drugs simply are not recommended for use during pregnancy and lactation. This places the burden on health care providers to weigh the potential benefits and risks in prescribing drugs for pregnant and breastfeeding women who become sick or may need to continue treatment for a chronic illness.
“It’s very frustrating as a clinician when you don’t have the data to tell a pregnant or breastfeeding patient whether something is safe for her to use,” adds Lisa Noguchi, Ph.D., epidemiologist, certified nurse-midwife and director of maternal newborn health at Jhpiego, the global health arm of Johns Hopkins University. “It creates a substantial gap in the services we are able to provide and comes at a real cost for women and children alike.”
Birth of a new approach
In 2006, Dr. Noguchi and Dr. Piper were part of a small team of experts who met to brainstorm how they could safely conduct a study of a biomedical HIV prevention product in pregnant women. The study they were discussing was to involve a gel formulation of tenofovir, a well-known HIV treatment drug that at the time was being evaluated in trials with women who were not pregnant or breastfeeding. Others at that meeting included Richard Beigi, M.D., an obstetrician and gynecologist from the University of Pittsburgh, now president of Magee-Womens Hospital of UPMC in Pittsburgh, and Heather Watts, M.D., director of HIV prevention, Office of the Global AIDS Coordinator, U.S. Department of State, then a medical officer with the Eunice Kennedy Shriver National Institute of Child Health and Human Development. 
The study they were strategizing about was a high priority for the new NIH-funded global research collaborative, the Microbicide Trials Network (MTN). It was only the second trial being planned by the MTN and was aptly named MTN-002. The mission of MTN – led by principal investigator Sharon Hillier, Ph.D., a microbiologist specializing in women’s health and infectious diseases at the University of Pittsburgh – is to evaluate microbicides, products applied inside the vagina and rectum to help prevent the sexual transmission of HIV. Jared Baeten, M.D., Ph.D., a global health expert from the University of Washington and also an advocate for research involving pregnant women, is MTN’s co-principal investigator.
Early on, Dr. Hillier became committed to prioritizing pregnant and breastfeeding women in HIV prevention research. In the 1990s, she closely followed the research of Taha E. Taha, Ph.D., a professor of epidemiology at Johns Hopkins University, who was among the first to report that pregnant women were particularly vulnerable to acquiring HIV.
The risk of HIV in these populations is now widely recognized, with estimates suggesting that women are two to three times more likely acquire HIV during pregnancy and four times more likely during periods of breastfeeding. For many women, the amount of time spent pregnant, breastfeeding, or both, represents a significant portion of their reproductive years when they are at increased HIV risk.
 “We knew from Taha Taha’s research that pregnancy was a time of heightened vulnerability to HIV,” says Dr. Hillier. “Still, hardly any studies of investigational products for prevention were being done in this population. Since the MTN was focused on testing topical products, we thought this would be a safer and more acceptable method for prevention, especially given the low level of systemic exposure to drugs provided by microbicides.”
“We knew from Taha Taha’s research that pregnancy was a time of heightened vulnerability to HIV,” says Dr. Hillier. “Still, hardly any studies of investigational products for prevention were being done in this population. Since the MTN was focused on testing topical products, we thought this would be a safer and more acceptable method for prevention, especially given the low level of systemic exposure to drugs provided by microbicides.”
When it comes to biomedical HIV prevention studies, women of reproductive age can enroll, but they are usually required to use contraception throughout study participation, explains Dr. Hillier. If they become pregnant, they must stop using the study drug immediately. These measures are primarily intended to protect the fetus or baby from potential harm, but also mean that little or no information about the safety of a drug during pregnancy or breastfeeding will be available. As a result, a drug that receives regulatory approval will be contraindicated for women who are pregnant or breastfeeding.
“Getting information in a controlled way through a research study is so much safer than approving a drug and just putting it out there for pregnant women to use,” says Dr. Piper, who practiced maternal-fetal medicine before joining DAIDS/NIAID. “The worst thing you want to see is pregnant women using a drug and then finding out there’s a problem.”
The MTN-002 team agreed that any potential risk from a small and controlled study was far less than the societal risk of excluding pregnant women from HIV prevention research entirely. They deliberated on the safest way to move the study forward. Tenofovir gel was a good candidate as there was reassuring safety data about it from animal studies and from registries that followed HIV-positive pregnant women who had used the drug in tablet form as HIV treatment.
 “We knew quite a bit about oral tenofovir in HIV-positive pregnant and breastfeeding women who were being treated, but MTN-002 was the first time we were proposing to evaluate it in HIV-negative women, and the first time it would be administered vaginally in a clinical study,” says Dr. Watts. “Given concerns about pregnancy safety, we devised a carefully laid out plan for the progression of a series of studies of the gel.”
“We knew quite a bit about oral tenofovir in HIV-positive pregnant and breastfeeding women who were being treated, but MTN-002 was the first time we were proposing to evaluate it in HIV-negative women, and the first time it would be administered vaginally in a clinical study,” says Dr. Watts. “Given concerns about pregnancy safety, we devised a carefully laid out plan for the progression of a series of studies of the gel.”
The study team decided to start with a single dose of tenofovir gel administered vaginally to 16 women within eight hours of scheduled cesarean delivery at one U.S.-based clinical site. This study design was approved by two institutional review boards and reviewed by the U.S. Food and Drug Administration (FDA), before proceeding. Finding the gel safe for both mothers and infants, the researchers designed a second study, MTN-008, in which two groups of women (a total of 90) in their third well as 15 women who were breastfeeding. In MTN-008, conducted at two U.S.-based clinical sites, the first group included women 37-39 weeks gestation who were randomized to receive tenofovir gel or a placebo gel, with the second group 34 -36 weeks gestation.
Essentially, the researchers employed a backward, stepwise approach – shifting the administration of gel from the time of delivery to earlier in pregnancy. In the MTN-008 study, they proceeded to the second group of women – who were earlier in their pregnancies – only after careful evaluation through an interim safety review.
Although tenofovir gel was found safe for the mothers and their infants in MTN-002 and MTN-008, it did not proceed to licensing after large trials found it was not effective for preventing HIV in women who were not pregnant or breastfeeding. Even so, the stepwise approach became the cornerstone of MTN studies in pregnancy and breastfeeding women. Indeed, MTN’s scientific portfolio in the intervening years has included a comprehensive program purposefully designed to take incremental steps for evaluating the safety of HIV prevention products in pregnant and breastfeeding women. Each study is carefully designed and implemented so that vital information can be collected while also ensuring the safety and well-being of women and their babies.
New studies and forward steps
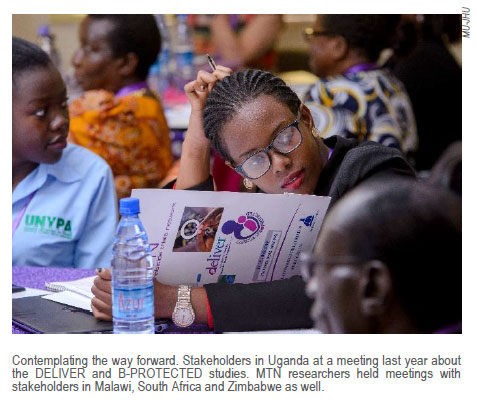
 Fast-forwarding to 2020 finds MTN-affiliated researchers busy implementing two major studies of the monthly dapivirine vaginal ring and Truvada® as daily PrEP in pregnant and breastfeeding women in Africa based on the approach identified by the MTN-002 team. DELIVER (MTN-042), for pregnant women, enrolled its first participant in February 2020, and B-PROTECTED (MTN-043), for women who are breastfeeding, is expected to start in the coming weeks. DELIVER is the first study of its kind in pregnant women, while B-PROTECTED is the first in women who are actively breastfeeding. (It follows an earlier study called MTN-029/IPM 039 that involved women who were still producing milk, but no longer nursing. See Pumped Up for HIV Prevention.)
Fast-forwarding to 2020 finds MTN-affiliated researchers busy implementing two major studies of the monthly dapivirine vaginal ring and Truvada® as daily PrEP in pregnant and breastfeeding women in Africa based on the approach identified by the MTN-002 team. DELIVER (MTN-042), for pregnant women, enrolled its first participant in February 2020, and B-PROTECTED (MTN-043), for women who are breastfeeding, is expected to start in the coming weeks. DELIVER is the first study of its kind in pregnant women, while B-PROTECTED is the first in women who are actively breastfeeding. (It follows an earlier study called MTN-029/IPM 039 that involved women who were still producing milk, but no longer nursing. See Pumped Up for HIV Prevention.)
These studies are vitally important for two reasons. First, Truvada as PrEP is approved for HIV prevention in many countries, but information about its safety in pregnant and breastfeeding women is limited. Second, the  monthly dapivirine vaginal ring is a new product currently under regulatory review, with much less known about its safety in these populations of women. Regulatory authorities and national programs will need specific information about safety to consider making these HIV prevention methods available to pregnant and breastfeeding women in the future.
monthly dapivirine vaginal ring is a new product currently under regulatory review, with much less known about its safety in these populations of women. Regulatory authorities and national programs will need specific information about safety to consider making these HIV prevention methods available to pregnant and breastfeeding women in the future.
MTN researchers also recently completed more than a decade-long observational study and data registry called MTN-016, or EMBRACE, in which women who unintentionally became pregnant in MTN’s larger studies and their babies were followed for a year. Mothers and infants from the MTN-002 and MTN-008 studies were also included. A total of 460 pregnant women and 413 infants participated in EMBRACE, which has provided invaluable information about the antiretroviral-based products used in MTN studies.
Thankfully, many other health experts are also recognizing the importance of including pregnant and breastfeeding women in research, with major research initiatives now dedicated to these populations. One such program called PHASES (Pregnancy & HIV/AIDS: Seeking Equitable Study), also funded by the NIH, is working to develop ethically responsible strategies for conducting HIV research in pregnancy. With a powerful motto, “Protection of pregnant women through research, not from research”, PHASES has benefited greatly from MTN’s vision, scientific innovation and significant accomplishments through the years, says Kristen Sullivan, Ph.D., project director of PHASES at the University of North Carolina.
Even so, says Dr. Beigi, when it comes to clinical trials related to epidemics, pregnant women continue to be excluded simply because the research is more scientifically complex. It requires leadership, support, dedication and funding to see through the many obstacles in planning and implementation. “You really need a group of people who care enough, and who are willing to rally around it and push the envelope,” says Dr. Beigi. “At MTN, we were all in complete agreement about the scientific imperative to do it, the public health imperative and the ethical imperative.”
 Dr. Hillier agrees. “You have to have advocacy from all sides to keep pregnant and breastfeeding women in the forefront of HIV research. You have to constantly define the risks and the benefits, and always be ready to recalibrate in the face of emerging data.”
Dr. Hillier agrees. “You have to have advocacy from all sides to keep pregnant and breastfeeding women in the forefront of HIV research. You have to constantly define the risks and the benefits, and always be ready to recalibrate in the face of emerging data.”
Most importantly, perhaps, you also need a good and trusted map to know where you’re going and the best way to get there. The foundation for conducting HIV research with pregnant and breastfeeding women used in the MTN-002 study continues to enable the safe collection of data in these populations today. By replacing guess work with evidence-based information, the field has taken a giant leap forward in giving pregnant and breastfeeding women the facts they need to make informed health decisions.
# # #
Click here for PDF version of this document.
See also
Pumped Up for HIV Prevention
